Hello all this is J. Mounika, a eighth semester student.This E Log depicts the patient centered approach to learning
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of “ patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
68 yr old male came to opd with chief complaints of difficulty in breathing and fever and since 1 day
* facial puffiness since yesterday morning
HOPI:
Patient was apparently asymptomatic 1 day back then he developed fever which is of low grade , intermittent relieved with medication ,associated with chills and rigor Associated with generalised body pains .
SOB since 5 hours which is sudden onset grade 3 not associated with chest pain, palpitations , pedal odema, decreased urine output
No c/o cough ,cold ,burning mitcturation, vomitings ,loose stools ,pain abdomen .
PAST HISTORY:
K/c/o htn since 1 yr on tab amlodipine 5 mg plus atenolol 50 mg po od .
Not k/c/o DM, asthma , TB, epilepsy, CVD
PERSONAL HISTORY:
He is married.
Mixed diet.
Appetite :Normal
Micturtion: normal
Bowel and bladder habits : normal
Sleep :Normal
Alcohol and smoking history: Drinks occasionally .
Smokes daily 10 beedis/ day stopped 15 days
FAMILY HISTORY:
No family h/o HTN, TB, heart disease,cancers, epilepsy.
GENERAL EXAMINATION :
Pt is conscious coherent cooperative well oriented with time place and person .
PALLOR : absent
ICTERUS : absent
CYANOSIS :Absent
CLUBBING :Absent
GENERALIZED LYMPADENOPATHY :Absent
ODEMA: Absent
Vitals:
Bp:150/80 mm of Hg
PR : 60 bpm
RR :22 cpm
Temp :97.3
SPo2 : At room air 74 % and 99 % at 6 litres of O2
Grbs: 116
SYSTEMIC EXAMINATION :
• No thrills and cardiac murmurs
RESPIRATORY SYSTEM:
• Dysponea present
* No wheezing
• Postion of trachea - central
• Breath sounds - Vesicular
* Adventitious sounds : Diffuse bilateral crepts present
ABDOMEN:
• Shape : scaphoid
• No tenderness, palpable mass, bruits
• No palpable liver and spleen
CNS:
• Conscious and coherent
• Speech - normal
No signs of meningeal irritation
• Glass gow coma scale - 15/15
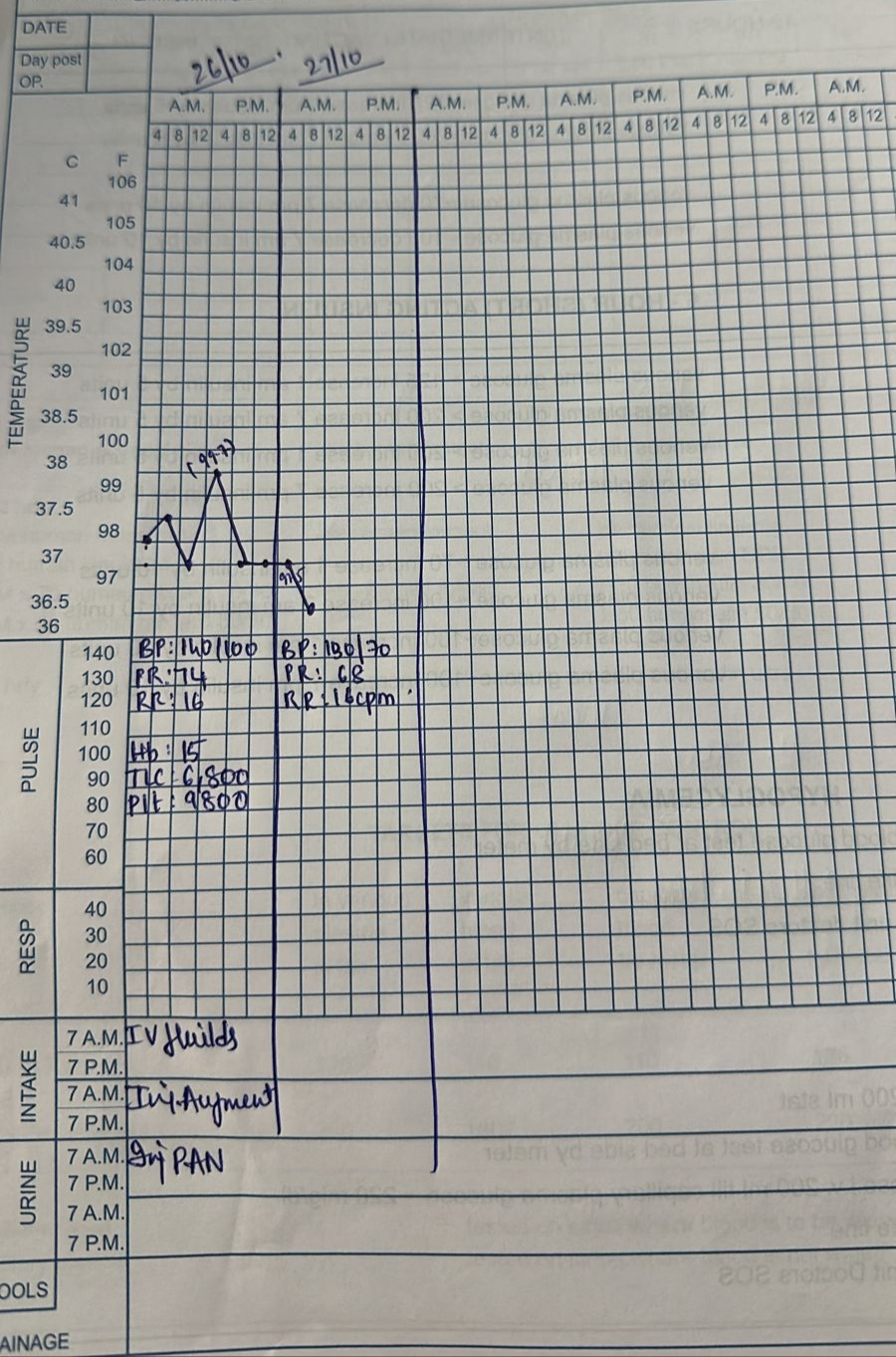
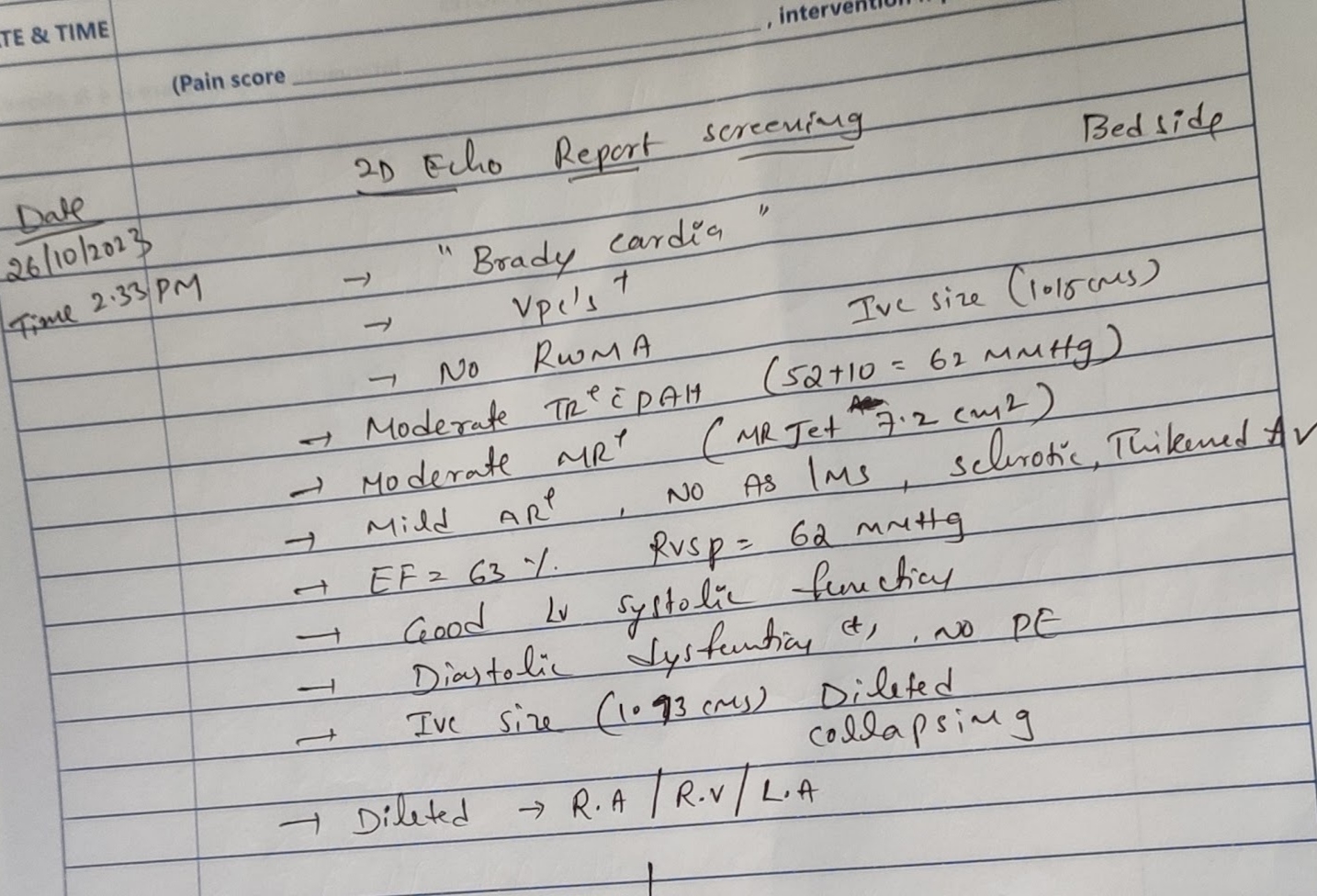
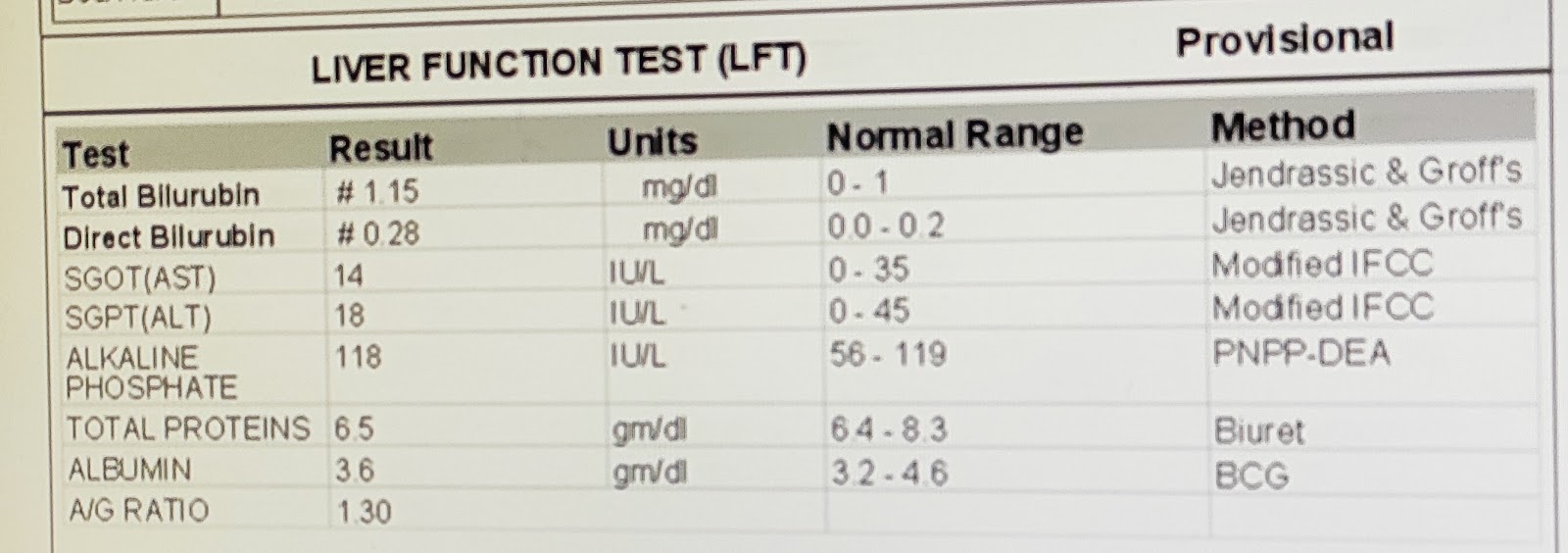
on 26/07/2023
on 27/10/2023
PROVISIONAL DIAGNOSIS: Pyrexia evaluation ( LRTI? COPD?)
TREATMENT: on 26/10/2023
Iv fluilds
INJ augmentin m 1.2 gm iv tid
INJpan 40 mg iv od bbf
INJ neomol 1gm iv/sos
Tab atorvastatin 20 mg po/hS
Tab ecosporin 75 mg po HS
TAB AZITHROMYCIN 500 mg po od
Tab oseltamavir 75 mg po bd











Comments
Post a Comment